Homelessness and Health
Homelessness isn’t just a housing issue. Struggling without a home usually also means struggling with poor health, and being unable to find enough support.
If asked what the three most important aspects of our lives are, most of us would say something like having reasonable health, somewhere comfortable to live and people we’re close to. But what happens if we have none of these? Poor health may rule out employment, which means having to rely on benefit payments, which limits what accommodation is affordable. And our health needs may mean that many types of housing are inaccessible or impractical. If we don’t have friends or family in a position to help, we would expect the health service, councils, and other organisations to provide a safety net. However, the support services industry has failed to provide for the complex needs of people with both health and housing problems. This is despite a definite relationship between homelessness and poor health. Research from St Mungo’s Broadway and Homeless Link found that 73 percent of homeless people have a physical health problem, and 80 percent have mental health issues (p.3, http://www.mungosbroadway.org.uk/documents/5390/5390.pdf). To what extent poor health is a cause or an effect of homelessness is hard to determine; for most homeless people, it’s probably both. What is clearer is that many people struggle to access often insufficient help from services lacking enough staff and resources.
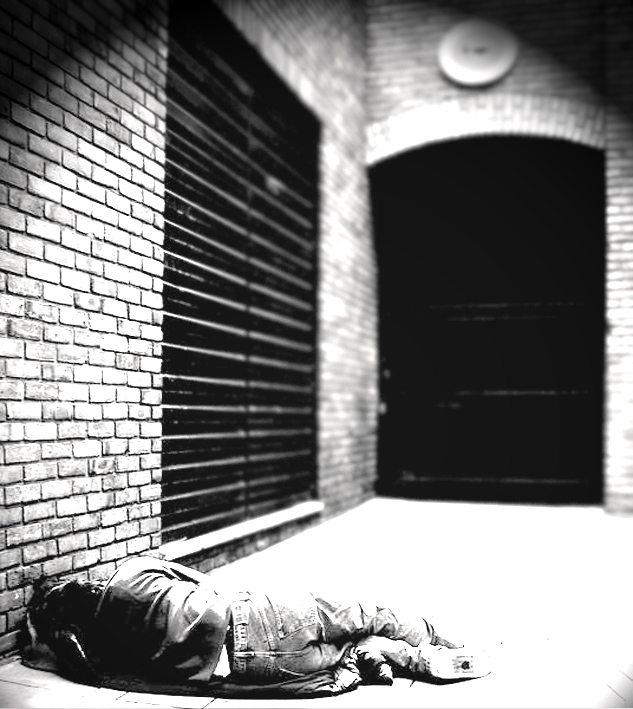
The definition of homelessness includes people in many different situations. The most extreme, and visible, aspect of homelessness is sleeping rough on the streets. A conservative estimate of the number of rough sleepers in England was 2,414 in 2013 (www.gov.uk/government/statistics/rough-sleeping-in-england-autumn-2013). Many more people are in various types of temporary housing, including homeless hostels, bed-and-breakfast accommodation, and staying with friends or relatives. Ten years ago, Crisis estimated that there were 380,000 of these ‘hidden homeless’, which is more than the total population of Leicester (p.3, www.crisis.org.uk/datafiles/publications/HHBIC_report%5B1%5D.pdf).
Despite their varying circumstances, all homeless people will have an unsettled way of life which exacerbates other problems, especially health. The most obvious, and stark, way of summing up the additional health concerns affecting homeless people is by looking at mortality rates. The average age at death of a homeless person is 47 years old, compared to 77 for the wider population. Homeless women, on average, live until they’re only 43, whereas in the wider population, women tend to live longer than men (p.2, Homelessness: A Silent Killer, Crisis, 2011).
One reason why homeless peoples’ wellbeing suffers is because of difficulties with accessing healthcare. Although there are no upfront charges to use NHS services, and prescription fees are waived for people on a low income, the bureaucracy of the NHS makes it hard for homeless people to navigate the system. The usual way to access healthcare is to make an appointment with your GP, who can then make referrals to hospitals or clinics for particular treatment. To register with a GP, you need a stable address, which creates the first barrier for homeless people. Without easy access to a GP, medical conditions could go undiagnosed or untreated. As a result, when a homeless person’s health deteriorates, they are more likely to approach a hospital directly.
A&E
Homeless people attend Accident & Emergency, or Casualty, departments six times more often than the general population (p.2, Healthcare for the Homeless, Deloitte Centre For Health Solutions, 2012). The numbers of homeless people attending A&E has been flagged up in the context of unbearable pressures on hospitals. The efficiency of A&E departments is measured against the government target of 95 percent of patients being treated within four hours, lowered from 98 percent in 2010. This winter, the mainstream media reported on how many hospitals have failed to meet this target. At the start of 2015, only 86.7 percent of patients in England were seen within four hours (BBC News, 14/1/15), with worse figures in other parts of the UK. Eight hospitals declared ‘major incidents’ because demand on A&E units had increased to more than could be managed.
The four hour target will be prominent in the minds of all A&E staff, alongside the stress of the excessive workload. The constant pressure to process patients quickly means that underlying health problems could be ignored. And the shortage of hospital beds means that not enough people will be admitted to a ward. Consequently, homeless people, especially rough sleepers, often get discharged from A&E straight back into a situation unlikely to promote their recovery. So, when their health deteriorates again, they will probably return to hospital in the near future. People trapped in this cycle of needing to go back to A&E again and again are called ‘frequent flyers’. One in ten homeless people use A&E at least once a month (p.5, Healthcare for the Homeless, Deloitte Centre For Health Solutions, 2012), with some returning partly because they have nowhere else to go, and a hospital is somewhere warm, dry and reassuring.
Not all homeless people who come in to hospital fit this profile of repeat visitors not registered at a GP, though. Lots of people first become homeless at the same time that they enter hospital, usually as the result of a crisis. If someone has had a stroke or an amputation, then it may not be possible or practical for them to return to their previous home. Or, the trauma of being evicted may have pushed someone to attempt suicide.
On the ward
If a homeless person is admitted into hospital, they’re likely to stay there three times longer than the general population (p.2, Healthcare for the Homeless, Deloitte Centre For Health Solutions, 2012). This is partly because homeless people – especially the long-term homeless – often have multiple and complicated health problems, particularly liver damage, asthma, pneumonia, tuberculosis, epilepsy, diabetes, malnourishment, trench foot, wound infection and blood-borne viruses like hepatitis C, especially among intravenous drug users. Drugs and alcohol are often used as a coping strategy by homeless people, and heavy use can lead to cirrhosis of the liver, infections and dependency. This creates a vicious cycle where homelessness both leads to and is prolonged by addiction. 40 percent of homeless heavy alcohol users believe that a lack of stable housing is the main barrier to their recovery. Over a third of homeless people die due to alcohol or drug misuse (p.2, Homelessness: A Silent Killer, Crisis, 2011). The crisis of becoming homeless or struggling with homelessness as a way of life is also often linked with mental health problems. Someone with depression or schizophrenia is less likely to fit in to the expected routines which come with having a job and a ‘normal’ lifestyle. As a result, they are often pushed into homelessness, which will exacerbate their condition.
Another reason why homeless people remain in hospital longer than average is delays in discharging them. The aim is for a patient to leave hospital when they’re judged ‘medically fit’ to do so. They may still need longer to recover, but they can do this in the reassuringly familiar surroundings of their own home. This isn’t going to be possible if the patient is homeless. There have been many instances of homeless people being discharged from hospital in a taxi straight to a council office or a hostel, with no prior notice. This is particularly unsettling for the person, who has left the hospital without knowing whether they will get anywhere to stay, at a time when their health still makes them vulnerable. The practice of wards discharging homeless patients in this way has become less accepted in recent years. However, if a ward doesn’t discharge a patient because they don’t have anywhere suitable to go, then this creates the problem of ‘bed blocking’. When someone who is medically fit to leave hospital remains in a hospital bed, it prevents someone else from having it and creates additional expense.
Discharged where?
If a patient needs to be discharged to a care home, a nurse would refer them to a social worker to make the necessary arrangements. But only people with severely reduced capabilities qualify for this assistance. Presumably, if hospital social services departments and care homes had more staff and resources, they would be able to support more people, and the criteria for accessing them could be relaxed. As the situation is at the moment, many homeless people who would benefit from social services assistance aren’t eligible. Instead, it’s usually left to nurses to try and find accommodation to discharge a homeless person to. They may approach the local council, although the criteria for qualifying for statutory assistance excludes many single people except those judged extremely vulnerable. Even if a disabled homeless person is eligible for assistance under council criteria, then there still might not be anywhere appropriate for them. Temporary accommodation often means a placement in bed and breakfast accommodation, which is notoriously shabby and intimidating, and unsuitable for someone with poor mobility or little resilience. Council staff are aware that they are working within a frugal, inadequate system, and will try to compensate by interpreting their guidelines broadly and with some sympathy. So, temporary accommodation may be arranged in empty flats, care homes or hotels.
If there isn’t an arrangement with the council, or if the homeless patient doesn’t qualify for assistance from them, then the usual option would be direct access hostel accommodation. However, hostels can be almost as intimidating as bed and breakfasts, and are unlikely to be accessible for disabled people. They may have stairs, shared bathrooms and kitchens which could make them unsuitable. If someone can get into a hostel, then they would usually be able to stay there until they can find long-term housing, such as a flat rented from the council or a housing association. This could still take many months, but at least they would have the benefit of staff support.
If a homeless patient is in the country unofficially and has no recourse to public funds, councils and housing providers are very unlikely to help. Not being able to claim benefits or work legally will mean that they can’t afford rented accommodation, including hostels and B&Bs, and will be left destitute.
Generally, the worse someone’s health is, the harder it is for them to get suitable accommodation, especially at short notice. The situation is eased once someone turns 55, as this is the age that sheltered housing usually becomes available. But for younger people, unless they have a profoundly limiting disability which makes them eligible for statutory support, there is very little available. In other words, there is a lack of accommodation for people whose needs are too high for usual homeless provision but too low for social services involvement. The types of people that would be worst affected by this gap in services are those who have had strokes, amputations, suicide attempts, a diagnosis of schizophrenia, or drug and alcohol addiction. Most would also suffer from depression.
The bottom line
Costs accrued by bed blocking and the complex medical issues of homeless people mean that the average cost of a hospital stay for a homeless person is nearly five times higher than that for other people. More precisely, a homeless person will cost the NHS almost £1,900 per hospital stay on average, compared with £391 for the general population (p.6, Healthcare for the Homeless, Deloitte Centre For Health Solutions, 2012). The NHS is always being pushed to reduce its spending to cope with funding cuts. So, it was recognised that investing in more support for homeless patients would reduce costs in the long run. Looked at this way, the homeless are an economic problem, rather than people in need. In 2013, the government announced funding of £10 million to improve support for homeless people being discharged from English hospitals. This involved recruiting specialist staff to arrange discharges into suitable accommodation with ongoing support. This led to reductions in both bed-blocking and frequent flyers. But this wasn’t enough for funding to be extended, and many of these services are no longer running. The solution was only temporary.
To some extent, a society can be judged on how well it treats its most vulnerable people. The problem of homelessness only arises in a society where adequate housing is only available to those who can afford it and, as we’ve seen, people with poor health face additional barriers. These difficulties reflect wider problems in society:
1. The bureaucracy of the NHS, councils and support services, which makes it hard for some people to access help in a more planned way. This problem can’t be solved just by ‘cutting red tape’ or simplifying procedures. The NHS, councils and support services all have to operate in the same economic market as any other institution, so they have to be run like any other. This involves bureaucracy to ration and restrict who qualifies to use them.
2. The lack of resources in hospitals, whether a shortage of beds, nurses, mental health staff, social workers or support workers. Again, this problem can’t be solved within capitalism because the economy can never support enough funding to meet everyone’s needs. Money tends to go where it can be re-invested to create more wealth, and the NHS isn’t an attractive investment for the elite. The economic downturn and climate of government spending cuts only highlight an ongoing problem.
3. The lack of accommodation which is both suitable for and available to disabled people. This is part of the overall housing shortage. It costs more to build or adapt accommodation for people with poor mobility, and landlords may be reluctant to invest the extra money if they don’t think it will end up profitable. When houses are built to be sold or rented, rather than because people need them, then anyone without enough money will struggle.
All of these problems are built in to the way our society is structured. When society is driven by economic forces, rather than what people want and need, then some people inevitably suffer. Increased funding, new services, or reformed procedures may help a few people in the short-term, but they can’t address the causes of the problem.
CLIVE HENDRY
